There's the meth-addicted baby born in Bristol, Tenn., who was approved for TennCare in January, but didn't get coverage until June.
There is the Knoxville mom who for seven months has dialed number after number trying to figure out the proper TennCare program to cover her adopted son who is blind, deaf and cannot walk. She keeps getting sent to HealthCare.gov, where she doesn't get clear answers. And she never gets called back.
The 65-year-old Knoxville woman who was told that she qualifies for a TennCare-based Medicare savings program - but continues to have her Social Security docked for the premiums that program was supposed to cover. No matter how many phone calls she makes, the problem doesn't get fixed.
These are just a few among hundreds of Tennesseans stuck in the limbo of a TennCare application process that federal officials have now decried in a harsh letter that states the agency is failing to follow federal law.
The clock is ticking for TennCare to address problems like a long-delayed $35 million computer system that was supposed to be used to determine TennCare eligibility.
The U.S. Centers for Medicare and Medicaid Services (CMS) is requiring the state to submit a plan to remedy its problems no later than Monday.
Tennessee health advocates are applauding the federal agency's decision to put TennCare officials on notice for a series of chronic problems. One expert called the June 27 letter "a severe rebuke" to an agency that has prided itself on being a national model in Medicaid cost-savings.
But TennCare officials indicated Wednesday that they are more likely to issue a rebuttal than a plan of action.
TennCare spokeswoman Kelly Gunderson said in an email that there are "numerous aspects of the letter with which we do not agree" and that the agency is working on its response to CMS. The agency has also said TennCare enrollment topped 90,000 this year, a record.
Dave Smith, spokesman for Tennessee Gov. Bill Haslam, deferred to TennCare's response on the matter.
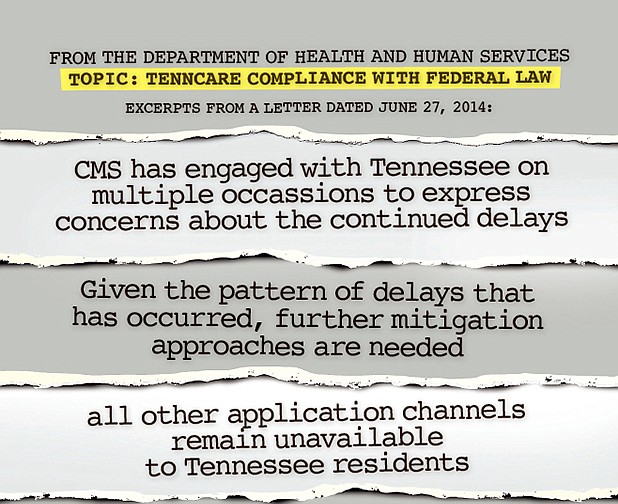
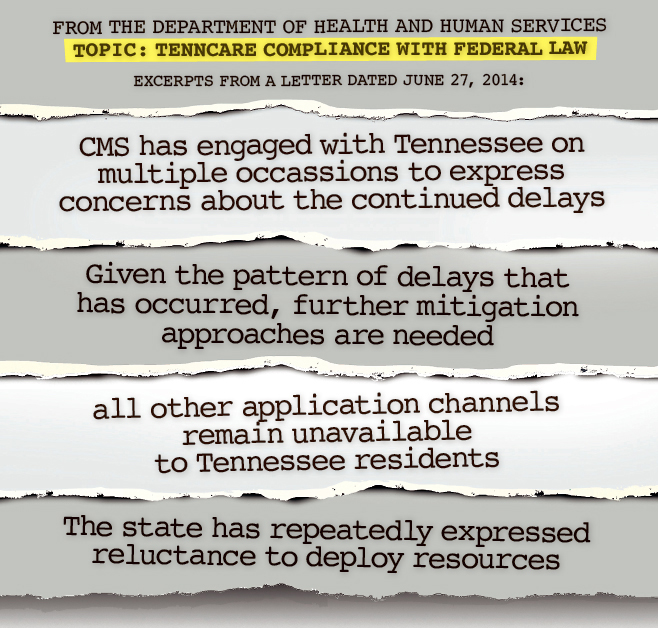
CMS Director Cindy Mann's letter to TennCare Commissioner Darin Gordon said federal officials said they have "engaged with Tennessee on multiple occasions" since last fall to express concerns about the unfinished computer system "and the downstream impact those delays are having on the state's ability to enroll eligible individuals in Medicaid."
Tennessee has "repeatedly expressed reluctance" to adopt effective solutions to cover the gap, Mann's letter said.
"We are the worst of the worst of all states on these factors," said Michele Johnson, director of the Tennessee Justice Center. The nonprofit public policy and advocacy group has for months been fielding calls from Tennesseans struggling with TennCare and meeting with the state agency to push for reforms.
"It's not about whether we hate Obamacare," she said. "This is about whether we are competent in running our own state-based system."
Walter Davis, director of the advocacy group Tennessee Health Care Coalition, said the federal action validates the group's long-held concerns.
Nevertheless, "it is not a happy day," he said.
"There needs to be some explanation of that and the resources they've put into it that aren't working," he said.
OUTLIER
When it comes to adjusting to new Medicaid rules, Tennessee has been an outlier in several ways.
It is the only state that does not have a state-based, in-person application process, and it is one of the only states that so far has not provided a way to let hospitals sign up needy patients in a process required by law that's known as "presumptive eligibility."
Though six states received similar letters from CMS about their failings, Tennessee's letter indicates that its level of compliance is worst among the group: It failed to meet all but one of "seven critical success factors" for implementing new Medicaid rules.
Many of those rules are based on a new system for determining Medicaid eligibility under the Affordable Care Act.
Instead of states using their own eligibility measures, they are expected to accept applications based on a federal measurement called the Modified Adjusted Gross Income, or MAGI.
To do that, Tennessee has been working on a $35 million computer system, known as the Tennessee Eligibility Determination System, or TEDS. The system, created by contractor Northrop Grumman, was supposed to be finished last fall, in time for the wave of new Medicaid applicants under the Affordable Care Act.
But it remains unfinished, and the state has most recently told federal officials the computer will not be ready until September of this year.
Because of this, TennCare has handed its application process over to HealthCare.gov - the only state to exclusively do that. People can no longer apply in person through the state's Department of Human Services.
That means hundreds of people seeking coverage through TennCare have struggled to navigate the web-based system, advocates say, or have become stuck in bureaucratic limbo as they're shuffled between state and federal hot lines.
Application files have backlogged in the transfers from federal to state systems and some applications seem to have been lost or forgotten.
"All other application channels remain unavailable to Tennessee residents and TEDS implementation continues to slip," wrote Mann.
Alice Weiss, program director for the Washington, D.C.-based National Academy for State Health Policy, explained that the seven factors referenced in the CMS letter are requirements for states to get funding for upgrades like TEDS.
The extent to which Tennessee has not met six out of seven of those factors "is of particular concern," Weiss said, calling into question whether Tennessee is abiding by ACA rules, but also standard Medicaid laws.
While CMS could potentially withhold funding from TennCare if it remained out of compliance, Weiss said the federal agency has not yet played that card.
"While [the letter] is a severe rebuke, it doesn't appear to be in a place where CMS is threatening that," Weiss said.
Aaron Albright, spokesman for CMS, said in an email that the federal agency will "remain in close contact" with states to monitor their progress in their enrollment systems and to ensure their updated mitigation plans and timelines are compliant.
Weiss said that regardless of the next steps, the public letter represents a turning point in the federal agency's conversations with the state.
"From this point, the public will be more involved in the conversation," she said.
Contact staff writer Kate Harrison at kharrison@timesfreepress.com or 423-757-6673.