Back surgery in 2001 left Connie Cook with a medical condition that she says sidelined her life - incontinence.
A stent in the kidney didn't help; neither did medication. Cook says she lost hope that her situation would ever improve. That is, until a few months ago when her doctor suggested pelvic therapy.
"When my doctor told me about it, I laughed," she says. "Nothing else had worked. I had never heard of pelvic therapy, but I was desperate and this was my last hope."
Cook's doctor sent her to Erin Shinkle, a Chattanooga-based physical therapist who specializes in pelvic health at Results Physiotherapy on Manufacturers Road.
"When my doctor sent me to Erin, I told her about my misgivings in pelvic therapy," says Cook, 60, of Chattanooga. "And, now, 12 weeks later, I'm basically cured."
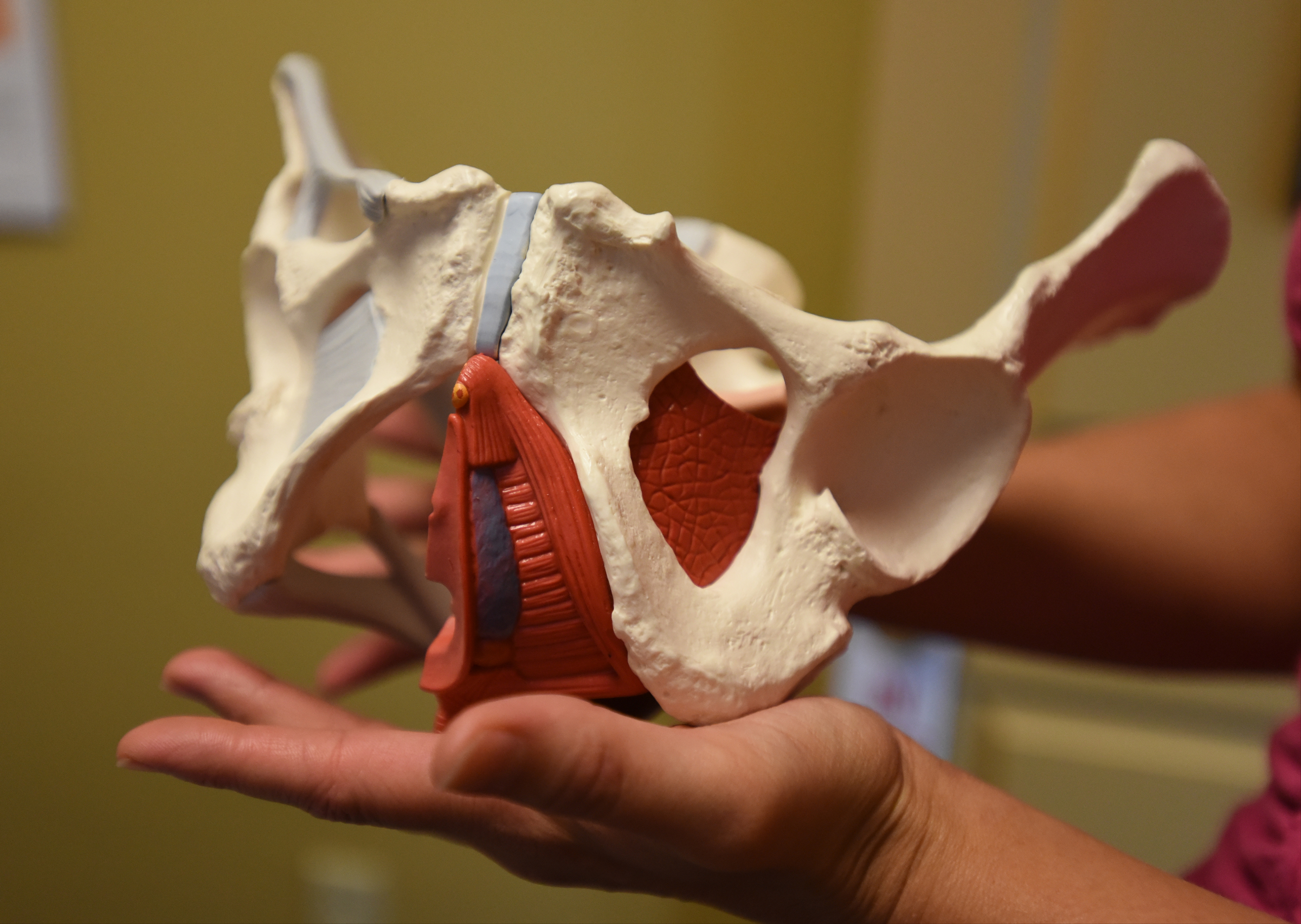
The therapy focuses on Kegels, an exercise that strengthens pelvic floor muscles. It's not a new discovery, says Shinkle, and the exercise can benefit both women and men.
"This specialty has been around for 40 years," Shinkle says. "Predominantly it's been completed by nursing as well as physical therapists and traditionally for incontinence. It has been evolving in the last few years."
The procedure "incorporates the whole aspect of the pelvic floor with the orthopedic considerations of posture, nerve involvement and musculature changes from the low back and hip regions," she continues. "We address many aspects of bowel, bladder and sexual health."
Patients who come to her often have diagnoses that include "chronic constipation, urinary or fecal leakage, pain with orgasm or intercourse, pain with pregnancy, postpartum issues of pain or leakage, post-abdominal/pelvic floor surgeries, low back and abdominal pain, she says.
Cook says the therapy has been life-changing for her.
"You just don't believe what you can learn to do with flexing your muscles in that area," Cook says. "It's the basic Kegel exercise, but I hold it longer than what's typical. I also stretch my stomach and back muscles.
"And the best part, I can do it anywhere. I can sit at the dinner table and do what I need to do. If I had known it would be this easy, I would have done it earlier."
Incontinence, in particular, is an age-old result of giving birth, says Shinkle, who attended undergrad and graduate school at Bellarmine University in Louisville, Ky., earning bachelor degrees in health science and a doctorate in physical therapy.
"Childbirth related changes such as C-sections, vaginal tearing, episiotomies and nerve compression can create a change in the function of the pelvic floor musculature and increased scar tissue can cause restrictions and pain," Shinkle explains.
"Most women consider it normal to experience leakage of urine and may continue to have pain in the pelvic floor area after delivery due to these changes. Adding the demands of lifting and caring for a child to a system that is already compromised from the tissue injury of childbirth can create an environment that leads to pain, urinary leakage and prolapse of the pelvic organs."
Most women don't realize, though, that the condition can be helped, even cured.
"The good news is that majority of these issues can be addressed with good pelvic health rehab," she says. "Why not address these issues head-on so that, in later years, you can not be afraid to jump on the trampoline with your child and, more importantly, maybe even avoid an unnecessary surgical procedure?"
For 14 years, Cook rarely left her house without wearing protection for urinary leaks.
"After my therapy with Erin, I drove to Florida by myself with no accidents," she says proudly. "I'm in Maine right now with my husband and I'm walking all over the place. No accidents.
"It's amazing - something so simple and it works, and I don't have to take medication. This was a godsend. I will keep doing the exercises for as long as I live. I don't want to risk things changing back to the way they were."
Shinkle says that, like Cook, people are surprised to learn that issues such as incontinence, constipation and back pain can be linked to the pelvic area.
"The pelvic floor muscles are very integral part of the structural support of the pelvis and low back," she says.
"I educate patients daily on how everything in the body is connected. I've even had patients who have had knee pain develop from hip weakness, which was associated with increased pelvic floor pain.
"The body is fascinating the way it adapts and changes movement in attempts to protect you. As a therapist, it is always important for us to treat the patient and not just the pain or problem, to make sure you address all the drivers that contribute to the movement adaptations," she says.
Shinkle, currently completing a Pelvic Rehabilitation Practitioner Certification through Herman and Wallace Pelvic Rehabilitation Institute, says men can also benefit from pelvic therapy; they have pelvises, as well, she says smiling.
"We see many men of various ages and different problems. Post-prostatectomy is a common diagnosis we see, along with urinary leakage, urinary frequency, urinary retention, pelvic pain in testicles and penis. These issues all correlate with the anatomy and function of the pelvic floor and may benefit from pelvic health rehab," she says.
And you don't have to go to your primary physician first to see her, Shinkle says.
"People do not need a doctor's referral to come in for an evaluation to see if it is a pelvic floor dysfunction," she says.
"And if they need further medical management or assessment, I do refer out to physicians."
Contact Karen Nazor Hill at khill@timesfreepress.com or 423-757-6396.