It is a common drama played out this time of year: A co-worker or spouse contracts the flu. Remaining on the offensive may mean a quick trip to the doctor's office, a flu test and a prescription.
But starting in January, Tennessee doctor's offices may not be able to offer flu tests or other common lab work at the same speed, ease or price as they have been.
The state's largest insurer, BlueCross BlueShield of Tennessee, has told doctors that it will cut reimbursements for lab tests by nearly half, covering 52 percent of what Medicare pays for lab tests instead of matching the Medicare reimbursement rate as it currently does.
The change means physician practices could soon bear more of the cost for a flu test, blood work, and any other kind of lab testing, or that patients could have to pay new bills for such work.
"Just to administer the flu test for Type A or B flu is much more expensive for us than the new reimbursement will be under BlueCross," said Laura Watkins, administrator of Chattanooga Family Practice Associates.
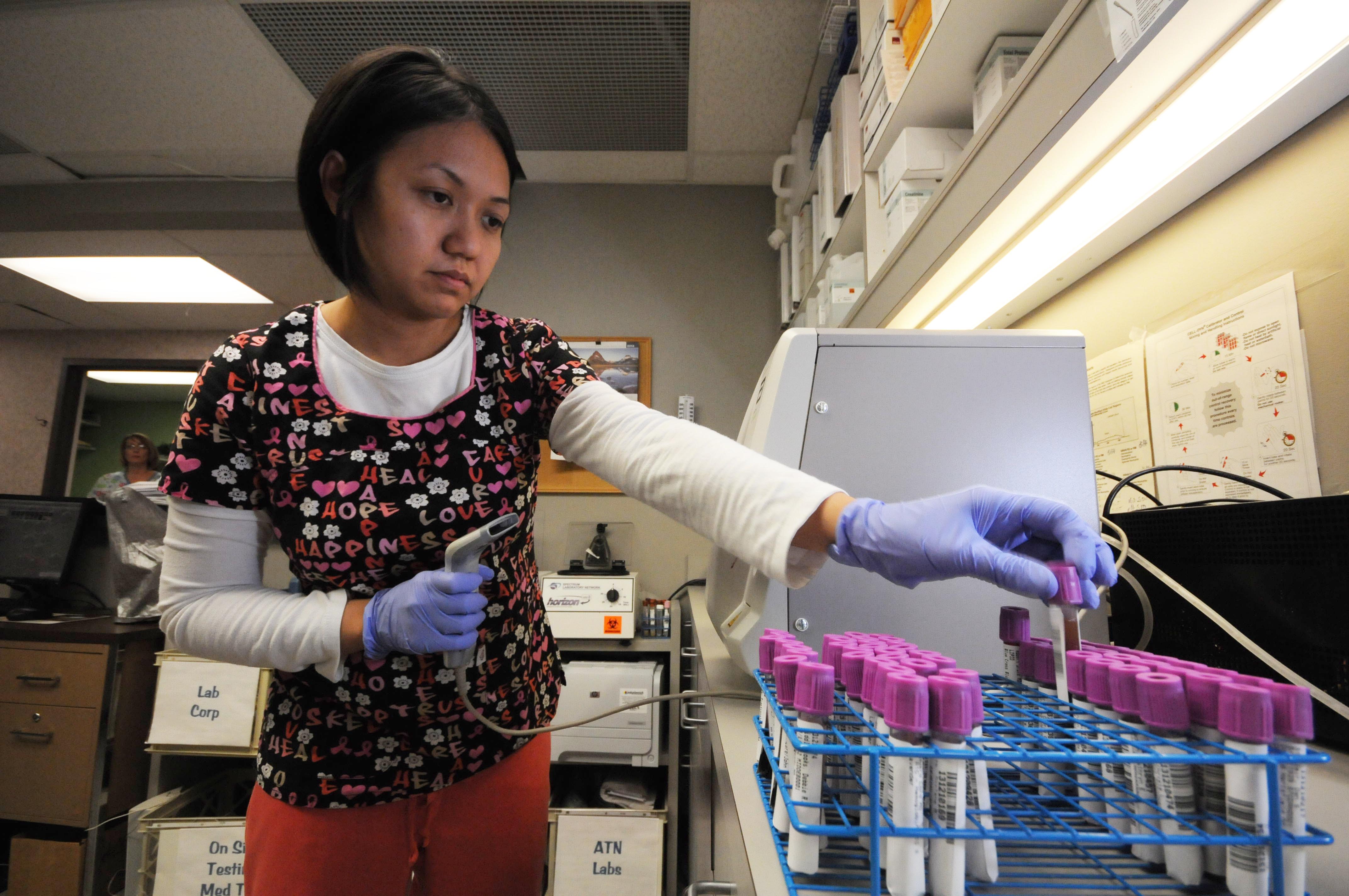
The practice sees up to 350 to 400 patients a day at its large primary care facility, and it does most of its lab work on site.
The office has just upgraded its lab equipment and has installed an electronic medical records system that integrates the lab results directly into the patient's chart.
But with the BlueCross announcement -- which does not affect hospitals or independent labs -- Watkins says the practice's standards for labs will change.
"The only thing we have left to do is notify the patient 'Your insurance may not pay for this test, and you may be responsible for the bill,'" she said. "In some cases, a patient may opt out of a crucial lab test because they do not want to pay the extra cost."
But the insurance company says its decision aligns with the current market rate for such lab work. The company has stated it does not want to be the lowest payer for these services, but we "do not intend to remain the highest."
"This is a move to make sure we're not continuing to pay above the market rate," said Gary Tanner, a spokesman for BlueCross. "In the long run it takes costs out of the system and makes health care more affordable for our members."
It also brings the company in line with its competitors, Tanner says.
"If anything, we were behind," he said.
But officials at the Tennessee Medical Association, which represents doctors in the state, say doctors don't see that.
"[BlueCross] feels their rates are higher than the national and the local level," said Phyllis Franklin, director of the insurance recovery program for the organization. "Our members don't necessarily agree with that statement."
Franklin said many of the doctors the organization works with are worried about the same challenges Watkins describes: Doctors' offices potentially losing money on labs, with reimbursements that will not cover the full cost of the tests.
Franklin said that will not necessarily mean higher costs passed along to patients, but it could mean more doctors outsource their lab work and require patients to go to a separate location for tests. That could result in separate billings.
Independent labs like Quest and LabCorp already receive the 52 percent reimbursement from BlueCross, prompting skepticism from some doctors and practices.
"We feel like this is a push to do away will physicians facilities and just contract with big labs," Watkins said.
Some health care analysts have identified overutilization of lab work and overcharging for the tests as consistent factors in rising health care costs.
But Tanner said the BlueCross decision to cut reimbursement is not based on that premise, but on lowering costs by sticking to market rates. The company will not be paying physicians anything less for seeing patients in its network, he said.
The insurer, which announced the rule in early November, has given doctors until Dec. 20 to reject the change, but has made clear that it reserves the option to terminate network status for doctors who do not agree to it.
Chattanooga Family Practice Associates plans to maintain its lab, Watkins said. But the office will have to make some major changes, potentially downsizing to make up for the extra costs.
"Come the new year, we're going to have losses until we figure out how we are going to make this work," Watkins said. "You can't turn these practices on a dime."
Contact staff writer Kate Harrison at kharrison@timesfreepres.com or 423-757-6673.