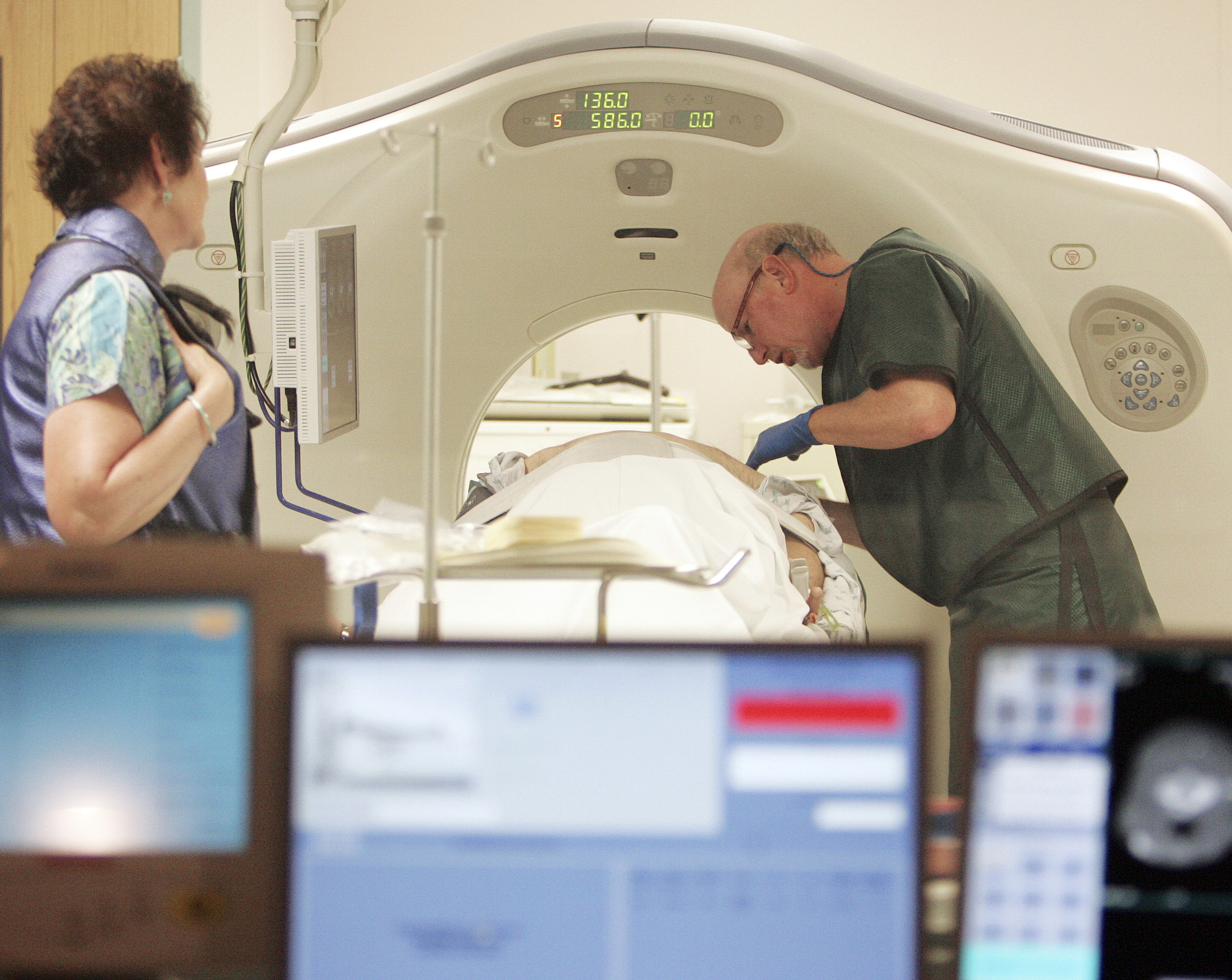
 Dr. Steven Birnbaum works with a patient in a CT scanner at Southern New Hampshire Medical Center in Nashua, N.H. For the first time, government advisers are recommending screening for lung cancer, saying certain current and former smokers should get annual scans to cut their chances of dying of the disease.
Dr. Steven Birnbaum works with a patient in a CT scanner at Southern New Hampshire Medical Center in Nashua, N.H. For the first time, government advisers are recommending screening for lung cancer, saying certain current and former smokers should get annual scans to cut their chances of dying of the disease.For the first time, government advisers are recommending screening for lung cancer, saying certain current and former heavy smokers should get annual scans to cut their chances of dying of the disease.
If it becomes final as expected, the advice by the U.S. Preventive Services Task Force would clear the way for insurers to cover CT scans, a type of X-ray, for those at greatest risk.
That would be people ages 55 through 79 who smoked a pack of cigarettes a day for 30 years or the equivalent, such as two packs a day for 15 years. Whether screening would help younger or lighter smokers isn't known, so scans are not advised for them. They also aren't for people who quit at least 15 years ago, or people too sick or frail to undergo cancer treatment.
"The evidence shows we can prevent a substantial number of lung cancer deaths by screening" -- about 20,000 of the 160,000 that occur each year in the United States, said Dr. Michael LeFevre, a task force leader and family physician at the University of Missouri.
Public comments will be taken until Aug. 26, then the panel will give its final advice. Reports on screening were published Monday in Annals of Internal Medicine.
The recommendation is a big deal for many reasons. The task force, an independent group of doctors appointed by the government, in recent years has urged less frequent screening for breast and cervical cancers, and no screening for prostate cancer, saying PSA blood tests do men more harm than good. There are no good ways to screen for ovarian cancer or other less common types.
But lung cancer is the top cancer killer worldwide. Nearly 90 percent of people who get it die from it, usually because it's found too late for treatment to succeed. About 85 percent of lung cancers in the U.S. are attributable to smoking, and about 37 percent of U.S. adults are current or former smokers. The task force estimates that 10 million Americans would fit the smoking and age criteria for screening.
The American Cancer Society used to recommend screening with ordinary chest X-rays but withdrew that advice in 1980 after studies showed they weren't saving lives. Since then, CT scans have come into wider use, and the society and other groups have endorsed their limited use for screening certain heavy smokers.
The scans cost $100 to as much as $400 and are not usually covered by Medicare or private insurers now. But under the new health care law, cancer screenings recommended by the task force are to be covered with no copays.
"It's generally going to be covered by all health plans" if the advice gets final task force approval, said Susan Pisano of the industry trade group America's Health Insurance Plans. She said her group may develop a response during the public comment period but has had "high regard" for the task force in the past "because they rely so heavily on the evidence" in crafting their recommendations.
The task force considered lung cancer screening in 2004 but said there was too little evidence to weigh risks and benefits. Since then, a major study found that screening the age group covered in the task force's recommendation could cut the chances of dying from lung cancer by up to 20 percent and from any cause by nearly 7 percent.
Screening "is absolutely not for everybody," not even all smokers, LeFevre stressed. That includes President Barack Obama, who said a couple years ago that he had quit smoking. Obama is too young (he will turn 52 in a few days) and too light a smoker (he reportedly smoked less than a pack a day), to be in the high-risk group advised to get screening.
The potential benefits of screening may not outweigh its possible harms for people not at high risk of developing lung cancer. A suspicious finding on a scan often leads to biopsies and other medical tests that have costs and complications of their own. The radiation from scans to look for cancer can raise the risk of developing the disease.
"These scans uncover things, often things that are not important. But you don't figure out that for a while," and only after entering "the medical vortex" of follow-up tests, said Dr. Peter Bach, a cancer screening expert at Memorial Sloan-Kettering Cancer Center in New York.
The best way to prevent lung cancer is to quit smoking or never start, and screening doesn't make smoking safer, doctors stress.
"That's everyone's public health concern: People will see this as a pass to continue smoking," Bach said of screening. "I don't think it's likely," because people know how harmful smoking is, he said.
