Tennessee Gov. Bill Haslam has joined “a steady drumbeat” of Republican governors who have recently proposed to expand their Medicaid programs after initially refusing to implement that part of the Affordable Care Act.
But Haslam’s proposal, dubbed Insure Tennessee, is still “a significant development” in the roll-out of health reform, said Joan Alker, executive director of the Georgetown University Center for Children and Families, who is an expert in Medicaid waivers like the one Haslam has introduced.
“It speaks to the fact that accepting the federal dollars and closing the coverage gap makes sense for every state,” Alker said. “You have more pragmatic Republicans saying we need to find a way to say yes to this.”
In an editorial board meeting Tuesday with Times Free Press reporters and editors, Haslam said the proposed program is not just a way to tap into the federal money offered through the Affordable Care Act.
He also wants the new model to reshape the state’s Medicaid program for the future.
“What we’d like this to do is to model what it will look like for the rest of the people covered by TennCare eventually,” Haslam said.
Haslam’s proposed changes, announced Monday, could expand health coverage to more than 200,000 uninsured Tennesseans who earn below 138 percent of the poverty level — $16,100 for an individual, or $27,300 for a family of three.
But Haslam does not want those new enrollees included in the current TennCare program, which covers 1.3 million people — children, pregnant mothers, caretakers of children and people with disabilities — and takes up a third of the state’s budget. The federal government will pay the entire cost of Medicaid expansion for the next two years, then 90 percent after that.
Read more
Lawmakers ready to look at Haslam Medicaid plan
Haslam said he wanted a plan that would “align incentives” to encourage health care providers and Medicaid users alike to improve health outcomes — a goal he said traditional Medicaid can’t deliver.
“We’re trying to put incentives in place for a population that gets free care and that cannot be denied care for any reason,” he said.
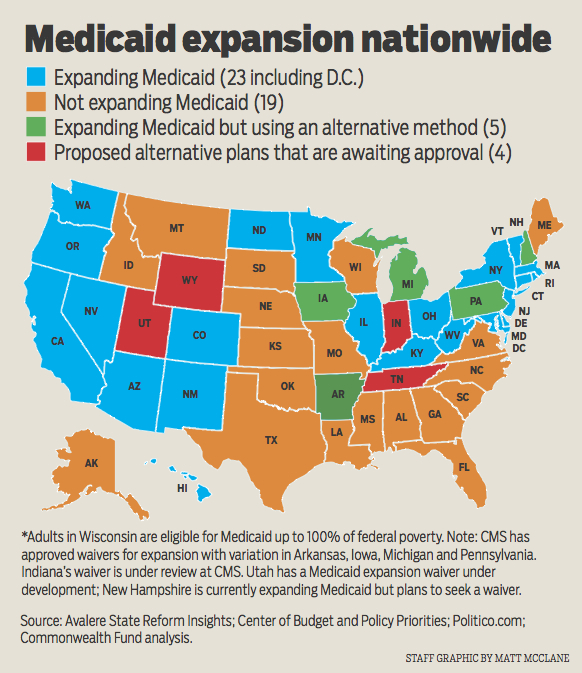
Of the 27 states that have expanded Medicaid under the health law so far, most opted for “traditional” expansion: Open up the current Medicaid program to everyone below 138 percent of the poverty level.
But Tennessee joins a handful of Republican-led states tailoring their own Medicaid expansion plans. The first was Arkansas, which is using the federal money to buy people private insurance. Dr. Wendy Long, the deputy director of TennCare, said Tennessee officials looked to the Arkansas model but did not find it cost-effective.
“What we found when we really explored that was that it would be more expensive than what we’re proposing here,” Long said.
Insure Tennessee borrows certain ideas from other states, but Haslam said the state crafted a unique, two-pronged proposal: A voucher program dubbed the “Volunteer Plan,” which helps people afford employer-offered health insurance; and a retooled Medicaid program called the “Healthy Incentives Plan.”
VOLUNTEER PLAN
The Volunteer Plan targets people who may have insurance available through their jobs, but who typically cannot afford it — people making around $8 an hour or less, Haslam said.
The Haslam administration estimates that more than half of those newly ensured under the expansion will fall into this category.
Employees could get vouchers toward their premium and deductible, with the amount capped at the figure TennCare traditionally pays to cover someone based on factors such as age. The voucher can only be used for employer insurance — not individual plans.
Long said the voucher plan has several advantages, such as potentially larger physician networks and member incentives. The goal, Haslam said, is to help people to transition fully to an employer plan.
However, Alker said private employer coverage typically costs more than vouchers would pay for.
HEALTHY INCENTIVES PLAN
The Healthy Incentives Plan will work more like traditional Medicaid, but will incorporate co-pays and premiums for singles who make more than $11,670 a year or $19,790 for a family of three.
But healthy choices may defray some of that cost. Health screenings, such as mammograms, or joining disease management programs for conditions like diabetes will earn workers credit to put toward health accounts.
“We have to make sure you’re rewarding positive behaviors and not penalizing things patients can’t do anything about,” said Long.
The Healthy Incentives Plan will insure people through TennCare’s existing, private-sector managed care organizations.
Long said co-pays will be “in the neighborhood” of $4 for an outpatient visit, $75 for inpatient hospital care and $8 for emergency room care. And all participants will have pharmacy co-pays, regardless of their income.
Contact staff writer Kate Harrison Belz at kbelz@timesfreepress.com or 423-757-6673.