A state official wants all health insurance companies in Tennessee to cover the costs of testing for the novel coronavirus, known as COVID-19, including waiving the copay and cost-sharing associated with the office or telemedicine visit.
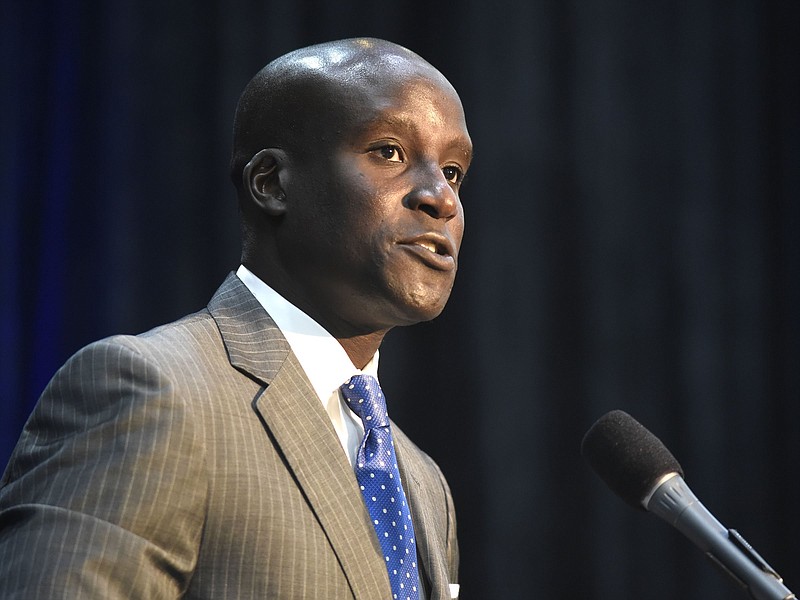
Tennessee Department of Commerce and Insurance Commissioner Hodgen Mainda said during a press call Monday that "cost should never be a barrier" to someone who's suspected to have coronavirus seeking medical care. The move is an effort to control the spread of the virus that as of Monday had infected at least four Tennesseans, Mainda told reporters.
"We do not want cost to be a hindrance or a barrier to someone who thinks they've got symptoms that are COVID-19 related," he said. "There's not a vaccine for this yet - it's new - and because [testing has] not been through the regular channels to get something approved, obviously it's costly."
While the move isn't a mandate, the department issued new guidance asking health carriers "to assist in combating this public health challenge" by waiving any out-of-pocket costs if a health care provider orders a COVID-19 laboratory test. In addition, the department wants insurers to waive the cost-sharing for an in-network provider office visit, an in-network urgent care center visit and an emergency room visit associated with the testing.
The guidance does not address surprise billing, which occurs when a person with health insurance unknowingly visits an out-of-network provider and gets hit with a large medical bill.
Mainda said that commercial testing for the virus would be available in the state as early as Monday afternoon.
Several insurance companies in Tennessee have already voluntarily adopted a similar policy, including the state's largest insurer, Chattanooga-based BlueCross BlueShield of Tennessee. BlueCross officials announced last week that the company would waive all member costs for coronavirus testing.
The new guidance also encourages the use of telemedicine - virtual doctors visits conducted through a computer or mobile device - to limit chances for the virus to spread in waiting rooms or at health clinics.
"Most, if not all, of the carriers have some sort of telemedicine in place for their covered lives," Mainda said. "We found this a much more effective and proactive way to try and combat the increased spread of COVID-19."
In addition to waiving the cost for coronavirus testing, the department requested that health insurers provide timely, accurate information, respond to consumer inquiries quickly and not use preauthorization requirements as a reason for not providing testing and treatment.
In a news release issued by the department, Tennessee's Assistant Insurance Commissioner Rachel Jrade-Rice urged Tennessee's health carriers to "make the overall safety and health of Tennesseans their priority to help prevent the spread of coronavirus.
"While this guidance may come at a cost to carriers, the risk of doing nothing carries too high a cost to Tennesseans and the country," Jrade-Rice said. "I urge Tennessee's health carriers to make the overall safety and health of Tennesseans their priority to help prevent the spread of coronavirus."
People with coronavirus symptoms - fever, coughing, shortness of breath - should contact their medical provider and stay away from others in order to prevent potential spread.
Contact Elizabeth Fite at efite@timesfreepress.com or 423-757-6673.