With in-person visits restricted by the coronavirus, getting medical advice or checkups on the phone or internet quickly gained in popularity this spring and proved effective enough that Tennessee's biggest health insurer has decided to make permanent its coverage of such telemedicine with in-network doctors and other health care professionals.
BlueCross BlueShield of Tennessee announced the policy change Thursday, becoming the first major insurer in the state to embrace telehealth for the long-term after the dramatic expansion of such care during the COVID-19 pandemic.
The Chattanooga-based health insurer began covering telephone and video visits with in-network providers in March when the Centers for Disease Management suggested that people keep at least 6 feet apart, wherever possible, to limit the spread of the COVID-19 virus. The change to cover virtual medical visits and care by BlueCross initially included primary care providers, specialists and behavioral health providers and was later expanded to include occupational, physical and speech therapy as well as ABA therapy services. All of these services will now be covered on an ongoing basis.
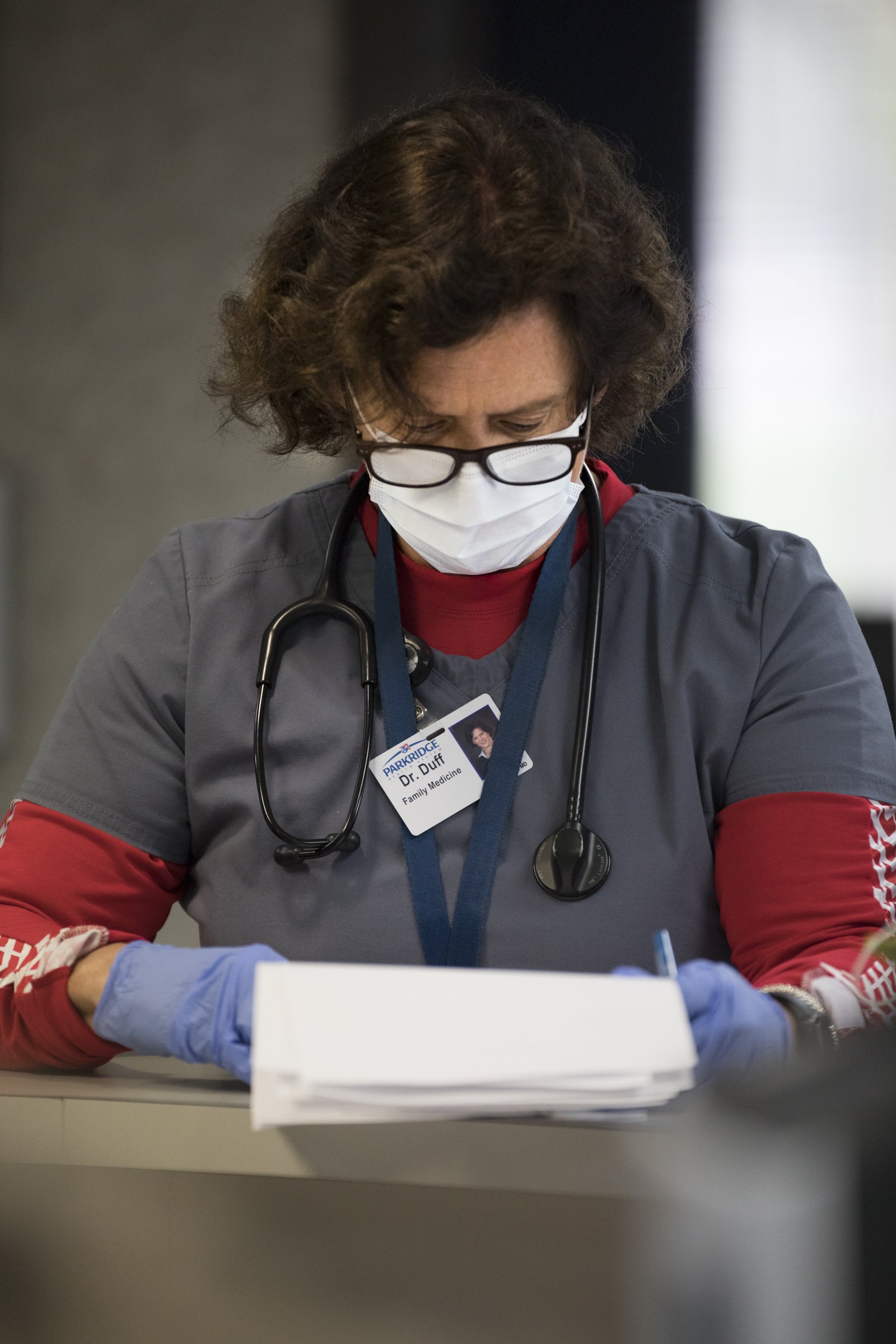 Staff photo by Troy Stolt / Dr. Siobhan Duff reads through a patient's chart before going on a telemedicine call inside of Chattanooga Family Practice on Thursday, March 26, 2020 in East Ridge, Tenn. Chattanooga Family Practice made the decision to convert all patient-doctor interaction to telemedicine calls for at least 14 days or until the practice could guarantee the safety of staff members through a higher availability of Personal Protective Equipment and Testing,
Staff photo by Troy Stolt / Dr. Siobhan Duff reads through a patient's chart before going on a telemedicine call inside of Chattanooga Family Practice on Thursday, March 26, 2020 in East Ridge, Tenn. Chattanooga Family Practice made the decision to convert all patient-doctor interaction to telemedicine calls for at least 14 days or until the practice could guarantee the safety of staff members through a higher availability of Personal Protective Equipment and Testing,"This recent period has proven virtual care can work for preventive, routine and maintenance care, and we're making this decision because the added convenience can bring better health," BlueCross CEO JD Hickey said in an announcement of the permanent change in its coverage of remote or distance healthcare visits.
BlueCross telehealth usage jumped across Tennessee in response to the coronavirus. From March 16 to April 14, the insurer managed 71,000 telehealth claims for its members - 18 times more than the number of claims submitted during the same time period in 2019.
Several major health insurers, including Humana, Cigna and Aetna in addition to many Blue Cross plans, have expanded telehealth coverage during the COVID-19 pandemic. Some states such as California have ordered insurers to cover telehealth procedures during the pandemic.
Tennessee has not mandated such coverage, and state Sen. Paul Bailey, R-Sparta, the chairman of the Senate Commerce and Labor Committee, said Thursday he was encouraged by BlueCross's voluntary decision to embrace telehealth.
"During the legislative debate on telehealth, the Senate maintained that the free market would best determine how telehealth services would play out," Bailey said. "It is best that doctors, insurance providers, and patients define the value of these services, rather than rely on burdensome definitions mandated by the General Assembly."
Bailey said is he optimistic that other insurance carriers will follow BlueCross "to provide Tennesseans with cost-effective telehealth services that are readily available and safe."
Dr. Harish Manyam, chief of cardiology at Erlanger, said about 80% of the information a doctor gets during a typical in-person visit is what the patient tells them, which can also be gained by a telephone or video conversation.
"Obviously we still need to draw blood at some point; we still need to be able to take vitals," said Lathram. "Instead of you coming in and sitting in the waiting room, or waiting in the exam room, what we can do is do the encounter over our telehealth platform, and then at your convenience stop by, have a lab only, and get your blood drawn and leave."
Hickey said BlueCross has been investing to improve the virtual care experience for its members for several years, with a focus on partnerships with in-network primary care providers.
BlueCross investments have included clinical quality programs and innovation grants to help practices improve the member experience, including telehealth services and enhanced digital tools. In February, the insurer announced a joint venture with Sanitas, a Keralty company, to open eight primary care medical centers in Middle and West Tennessee.
"We can't fulfill our mission without clinicians," said Hickey. "And we're always looking for new ways to work together and bring better health to the people we serve together."
The company has also made its own PhysicianNow virtual services available at no cost for many members through June 30. Those visits will continue to be available with regular cost-sharing, and many BlueCross members also continue to have free access to 24/7 Nurseline services.
Emily Crisman contributed to this report.
Contact Dave Flessner at dflessner@timesfreepress.com or at 757-6340.
