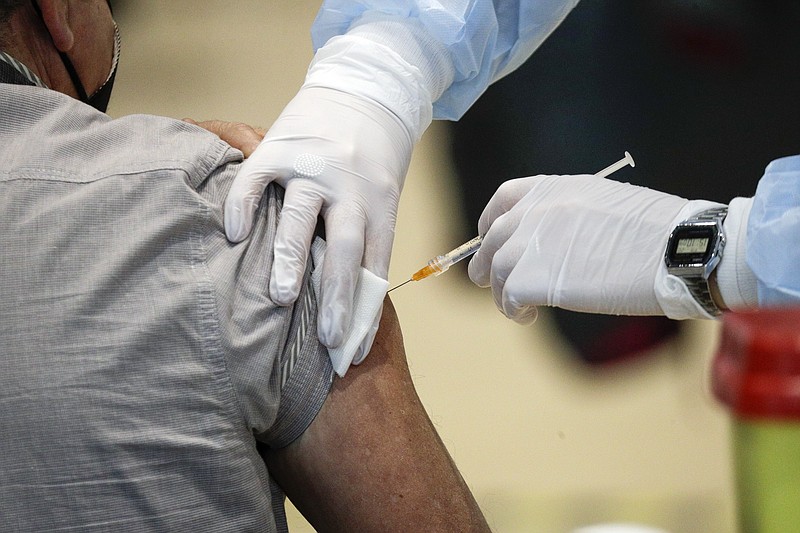
Tennessee's low COVID-19 vaccination rate threatens more than just those who choose not to get vaccinated, which is why the health care and scientific communities are pushing for more education and efforts to combat vaccine hesitancy in order to get more shots into arms.
"My grave concern is that if people don't appreciate the continued toll that this pandemic is taking on our country, and they don't recognize the benefits of vaccination, our ability to get to that state of so-called 'herd immunity' is uncertain," infectious disease specialist Dr. Jay Sizemore said during an Erlanger Health System Board of Trustees meeting Thursday.
"Herd immunity" occurs when a large enough portion of the population is immune to an infectious disease that it provides indirect protection to others who aren't immune. That's because circulation of the disease grinds to a halt when there aren't enough susceptible people left to infect.
Immunity can be achieved through vaccination or prior infection. However, vaccination is always preferred. Vaccines prevent more death, illness and opportunity for the disease to spread, and herd immunity for a disease has never been achieved without a vaccine.
The threshold for herd immunity differs by disease and depends on how infectious it is. Measles, one of the most contagious diseases in the world, requires about 95% of a population to be vaccinated, while the threshold for polio is about 80%, according to the World Health Organization.
Those thresholds are important, because some people will never be able to be vaccinated due to medical conditions, and those diseases will begin to resurface if vaccination levels dip below those rates.
In the year leading up to the pandemic, both measles and polio saw a resurgence worldwide due to a drop in vaccination rates.
Polio remains officially eradicated in the United States since 1979 thanks to a successful vaccination program, but there were nearly 1,300 cases of measles from Jan. 1, 2019, through Dec. 31 - the most cases in the U.S. in 27 years.
(READ MORE: Measles and other infections had a big year across U.S., Hamilton County)
Ability to achieve herd immunity also depends on how long immunity to a disease lasts. Even though measles is highly infectious, immunity lasts a lifetime, which makes the high bar of 95% vaccination rate attainable.
It's unknown how many people must be vaccinated against COVID-19 in order to reach herd immunity, but scientists estimate the threshold is around 70%.
Robert Bednarczyk, an assistant professor of global health at the Emory University Rollins School of Public Health, said it's more important to get as many people vaccinated as possible than to focus on a percentage. That's because other factors, such as population density and the vaccination levels of surrounding communities, all impact herd immunity.
"If you have 70% that are vaccinated that are living in one small area of a county, and the other larger parts of that county are remaining unvaccinated, that's a large cluster of people who are potentially at risk and they may not be reaping the benefits of that herd immunity," Bednarczyk said.
Though some portion of the population is protected from COVID-19 through prior infection - a protection that lasts an estimated eight months and possibly longer - vaccination levels in the Chattanooga region are nowhere near close enough to achieve herd immunity.
Meigs County leads the region in vaccination rate with 17.4% of its population fully vaccinated, followed by Hamilton County at 14%. Grundy County's vaccination percentage is the lowest, with only 7.8% of the population fully vaccinated.
Still, Sizemore remains hopeful.
"I think we have the opportunity to achieve herd immunity," he said. "I think we've got a ways to go."
Contact Elizabeth Fite at efite@timesfreepress.com or follow her on Twitter @ecfite.