The Erlanger Board of Trustees' decision in October to remove the hospital's chief of staff is drawing concern from physicians even outside the health system. And well it should.
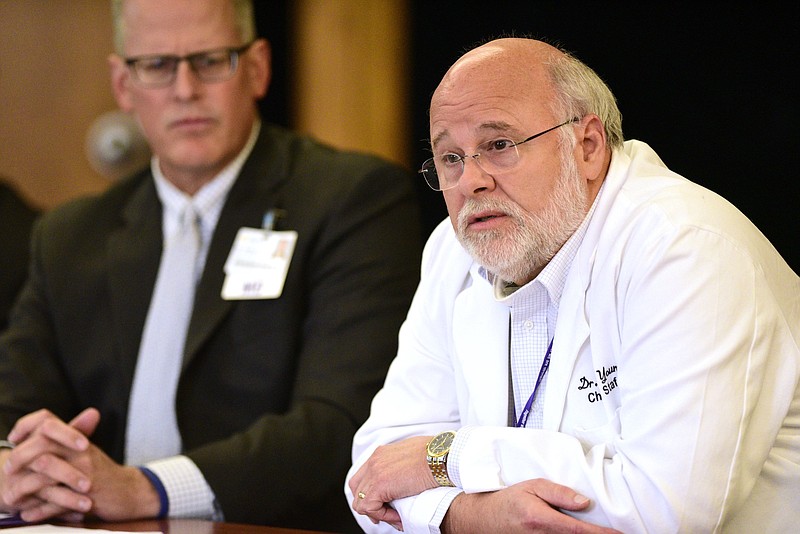
Trustees voted 6-3 to remove Dr. Chris Young, an anesthesiologist, from both his chief of staff position and his seat on Erlanger board itself. Young, a past president of the Tennessee Medical Association and longtime advocate for Erlanger who has practiced there for more than 30 years, spoke openly recently about the challenges the public hospital faces in a PBS "Frontline" and NPR documentary on the financial pressures faced by American hospitals serving low-income and uninsured patients. The show aired in May.
Five months later, his ouster was attributed by the board to allegations he shared unspecified confidential information - a claim that Young disputes. "I never improperly disclosed information I possessed solely by virtue of my duties as a board member," Young wrote in a letter sent to trustees.
One has to wonder if Erlanger's management and six of the hospital's trustees who voted to oust Young - none of them physicians or having other medical experience - are just embarrassed at the hospital's bottom line. And at the fact that hospital policy shifted to seek better paying patients. And at the fact that Young said Erlanger's future may come down to private investment.
Though the facility apparently is still eking out a small profit, its cushion is considerably behind those of other local for-profit and nonprofit hospitals.
Is Erlanger now simply looking for a scapegoat after the Frontline documentary made clear the financial challenges of "safety net hospitals" - those that serve all patients regardless of insurance status or ability to pay for care.
Clearly, doctors in town don't see Young's ouster the same way as those six trustees who voted Young off the island.
Fifteen physician leaders on the board of directors at the Chattanooga and Hamilton County Medical Society, which represents more than 1,000 area doctors in various practice settings with different hospital affiliations, last week sent trustees and Erlanger management a letter - obtained by the Times Free Press - saying the relationship between the board and Erlanger's organized medical staff has "become the topic of enormous concern and conversation" among physicians throughout the community.
"Our board of directors includes a diverse group of physicians who are profoundly concerned about the perceived loss of autonomy of employed and independent medical staffs, compelling us to document our concerns," the letter states. "This situation is heightened because the physician in question is without a doubt one of the most widely respected physician leaders in the state and has voluntarily devoted his time and much of his career to the Erlanger Health System."
The Frontline documentary called attention to a long-brewing crisis in American health care brought to the forefront by the COVID-19 pandemic - the jeopardized future of many safety-net hospitals like Erlanger.
The documentary featured several leading Erlanger physicians and former U.S. Sen. and Chattanooga Mayor Bob Corker, all calling out the need for a pathway to financial sustainability for Erlanger.
Frontline analyzed annual hospital filings and obtained supplemental payment information from the state Medicaid agency, TennCare. Looking at data covering 2015 to 2019, Frontline used an analytical methodology used by numerous Medicaid experts and found that for six Tennessee hospitals designated as safety nets, the uncompensated costs of caring for Medicaid and uninsured patients increased by 31%. But the supplemental payments through TennCare and the Medicaid only increased by 5%.
At the same time, Frontline saw that some for-profit and not-for-profit hospitals received much greater increases in supplemental payments. Frontline said Medicaid officials in Washington and Tennessee would not agree to an interview. Instead, TennCare officials for Tennessee, one of 12 states that has refused to expand Medicaid under the Affordable Care Act, told Frontline in a statement that the disparity its journalists found "is not reliable" because it does not take into account key factors like care provided out of state patients.
Raise your hand if you think people flock to the Volunteer State for free hospital care?
Frontline found that Erlanger's cost of caring for uninsured and under-insured patients jumped 53%, but its supplemental payments from the state and federal governments only rose 3.6%.
That disparity - and learning that for-profit and not-for-profit hospitals were getting more supplemental payments than Erlanger - doesn't surprise us. Last month we learned that federal auditors had analyzed $2 billion in certified public expenditures Tennessee claimed from 2009 to 2014. That audit found that the state may have to repay the federal government some $767.5 million in "excessive" payments.
The auditors' report noted the reason for the federal deep dive: The state claimed the same amount, $373.8 million, for fiscal years 2010 through 2013. Really? The exact same amount even as health care was costing more and more?
Clearly the state - and perhaps Erlanger, too - is falling down on the job on overseeing our health care - both our health care needs and our overly complicated health care dollar management.