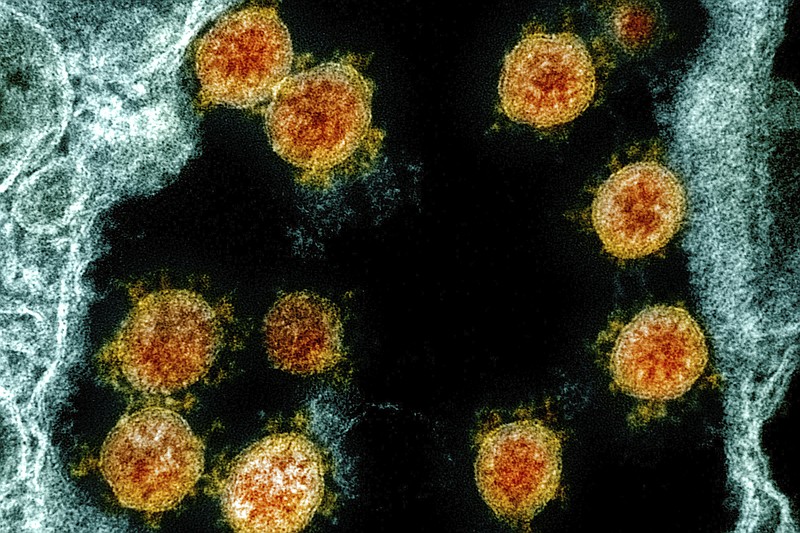
Hopes for arresting the Covid-19 pandemic, caused by the novel SARS-CoV-2 virus, rest upon development of an effective vaccine. Accelerated research to develop a specific vaccine is underway in dozens of companies and institutes in several countries.
Even before the current pandemic erupted, the Coalition for Epidemic Preparedness Initiatives (CEPI) had been launched in 2017 to study existing epidemic diseases such as HIV, and to prepare for "disease X," an undiscovered, viral threat to world health. CEPI supported development of new methods to design and mass produce vaccines so that a system would be in place when "disease X" erupted. The Bill and Melinda Gates Foundation contributed $460 million to co-found CEPI, which was also supported by London-based Wellcome Trust and a consortium of nations except the U.S.
Traditional methods for development of a vaccine for a viral illness involve years of research, development and testing. Viruses are grown on eggs or in cultures of cells. A typical vaccine includes either killed or weakened viruses. Some vaccines, such as polio vaccine, provide years of protection. Others, such as the influenza vaccine, require yearly boosters to deal with virus mutations. CEPI and other research institutes developed more rapid methods to produce synthetic vaccines.
On Jan. 12, China shared the genetic sequence of the new virus, subsequently named SARS-CoV-2. Think of this genetic information as a blueprint for the virus. With this information, scientific laboratories succeeded in making copies of parts of the new virus within weeks. A copy, or antigen, forms the basis of a new vaccine.
If a vaccine is effective, it will stimulate the body's immune system to form antibodies to neutralize the antigen. The immune system stores this information so that antibodies are promptly produced and released when the body is invaded by the virus for which the vaccine was created. Dozens of clinical trials of potential vaccines are underway.
A new vaccine is first tested in animals to determine if the animal develops antibodies to the injected material. The first human trial involves a small group of volunteers to determine if it is safe and if it leads to the production of antibodies against the virus. Different concentrations of vaccine may be used at this stage of testing to determine the smallest dose that will be effective.
In the second phase of human testing, a vaccine is given to a larger, more diverse volunteer group to evaluate in more detail its safety and effectiveness. Because of the COVID-19 pandemic, several different vaccines might have to be evaluated simultaneously in different groups of people to determine which is safest and most effective. Vaccine trials would also have to determine if a single dose or two doses is required to confer immunity. Follow-up studies would ascertain if yearly booster shots are necessary and to identify any unexpected, long-term side effects.
Estimates of when a SARS-CoV-2 vaccine will be available range from six to 18 months.
In anticipation of the need to mass produce the new vaccine, the Gates Foundation is funding the construction of seven factories, which will be ready when the best vaccine is identified.
Ethical questions should be addressed now:
* If an effective vaccine is developed in one country, will the vaccine be immediately shared worldwide or used exclusively in the country of its origin?
* Within a country, who will determine priorities for receiving the new vaccine?
* Who will pay for the manufacture and distribution of the vaccine? Who will pay for individual doses, especially for poor and underserved populations in our country?
* Who will oversee the distribution and administration of the new vaccine to poor nations with limited health care systems? Because viral vaccines often need to be frozen until the time of administration, this is a complex problem.
Contact Clif Cleaveland at ccleaveland@timesfreepress.com.